Voice Recognition Technology in Healthcare: Benefits for Patients and Providers
Explore how voice recognition technology is being used across healthcare and the role of voice assistants in clinical environments.
Continue Reading
There is no doubt in the fact that the healthcare industry is going through a rapid digital transformation by frequently coming up with new technology for patient care.
Whether it is hospitals, clinics, or other healthcare institutions, each can now rely on technology to effectively manage patient data, streamline workflows, and deliver better care.
Among these helpful technological tools for healthcare are EHR (Electronic Health Records) and EMR (Electronic Medical Records) systems, too. Understanding the difference between EHR vs EMR development is essential for healthcare organizations looking to build the right digital foundation.
At first, these two terms might sound similar as they both are used to digitize patient information and replace paper charts, but in practice, the difference between these two is that they serve different purposes and have unique strengths.
Looking to choose between the two?
It all depends on your healthcare organization’s size, goals, and how you plan to manage patient data long term.
Let’s make it simpler: an EHR system is built for broader data sharing and interoperability across multiple healthcare entities, while an EMR system is designed mainly for managing patient information within a single practice. Each system offers valuable benefits.
But what if you select the wrong one?
This might limit scalability, collaboration, and even compromise compliance in your healthcare institution.
Let’s explore everything you need to know about EHR vs EMR Development, from what each system does to its key applications, advantages, and how to decide which one fits your healthcare business.
An EMR system is basically a digital version of a patient’s paper chart, which is used within a single healthcare facility, like a doctor’s office, clinic, or hospital department. It contains detailed patient data such as medical history, diagnoses, lab results, prescriptions, allergies, and treatment plans.
You can think of it as the internal memory of a healthcare process. From visits, prescriptions, to lab tests, everything is recorded and stored in the EMR. The system helps doctors and staff track patient progress over time, and it can also identify when checkups or screenings are due, and ensure no important details are being missed.
So what’s the catch?
EMRs are practice-specific, which means that the data typically doesn’t travel outside the organization. So, for example, if a patient is switching to another hospital or choosing to get the rest of their treatment from some other doctor, the records would need to be printed and exported manually. This limited interoperability is what differentiates EMRs from EHRs.
Despite this limitation in the EMR system, it can be a very important step in digitizing the healthcare institution. It offers a centralized, organized, and secure way to handle patient data, reducing paperwork. This minimized human error and allowed clinicians to make quicker and more informed decisions.
From a development point of view, EMR software focuses on improving the internal workflows. If we look at the broader EHR vs EMR development landscape, EMRs serve as the first step toward digital transformation. The goal in this system is to make the process of recording, accessing, and managing patient data intuitive and efficient for healthcare providers. A well-built EMR system will not just store information; it will also help medical staff take action on it.
An EHR system is a step beyond the EMR. While EMRs are designed for use within one healthcare practice, EHRs are built for interoperability, meaning they allow patient information to be shared securely across different hospitals, clinics, pharmacies, and laboratories.
In simpler terms, if EMRs are about “your clinic’s data,” EHRs are about “the patient’s entire medical story.”
An EHR includes everything found in an EMR, including medical history, medications, allergies, and test results, but it also integrates information from multiple care providers. This creates a comprehensive, real-time view of a patient’s health that can be accessed by authorized healthcare professionals anywhere the patient receives treatment.
Here’s what makes EHRs critical for modern healthcare systems:
From a development perspective, EHR systems are more complex and scalable than EMRs. They require robust security frameworks, regulatory compliance (such as HIPAA), and advanced data exchange protocols (like HL7 or FHIR).
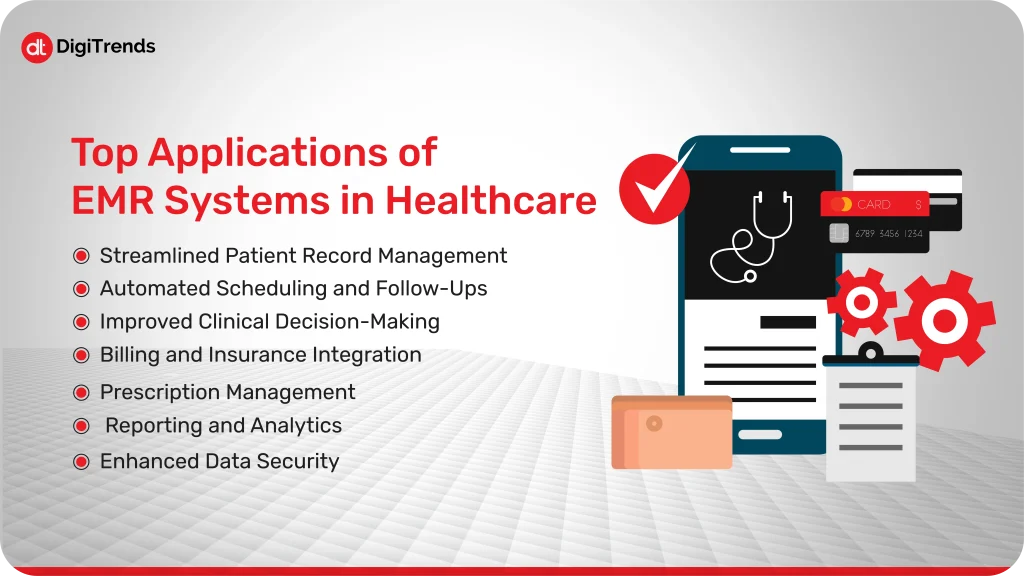
EMR systems have become a core part of modern clinical practice. In the context of EHR vs EMR development, EMRs represent the foundational layer that most healthcare providers start with before scaling to connected systems.
EMR systems have become a core part of modern clinical practice. They simplify day-to-day operations and make patient care more precise, consistent, and data-driven. Here are the key ways healthcare organizations use EMRs to improve their workflows and decision-making.
Instead of dealing with paper charts, every patient’s record is stored in a secure, centralized database. Physicians and nurses can access complete patient histories instantly, past diagnoses, allergies, lab results, and prescriptions, all in one place.
This not only saves time but also reduces the risk of lost or incomplete files. It’s especially useful in high-volume clinics where staff need quick access to accurate patient data.
EMR systems integrate appointment scheduling and patient tracking into one platform. They automatically flag follow-ups, vaccination schedules, or chronic disease check-ins.
For example, if a diabetic patient is due for a checkup, the system can trigger reminders for both the doctor and the patient. This kind of automation ensures better continuity of care without depending solely on manual tracking.
EMRs often include clinical decision support tools, which analyze data to alert physicians to potential drug interactions, allergies, or abnormal lab values.
These real-time alerts improve diagnostic accuracy and treatment safety, especially in busy environments where human oversight can easily happen.
Many EMR systems are integrated with billing modules and insurance verification tools. As soon as a doctor enters a diagnosis or procedure code, the system can automatically generate claims or update billing records.
This integration reduces administrative burden, minimizes coding errors, and speeds up the reimbursement cycle, an essential advantage for private clinics and hospitals managing tight cash flows.
Electronic prescribing (e-prescribing) is one of the most widely used EMR features. Physicians can send prescriptions directly to pharmacies, eliminating handwritten errors and improving medication tracking.
It also allows doctors to view a patient’s medication history, making it easier to avoid duplications or harmful drug combinations.
Beyond clinical use, EMR systems collect valuable data that can be analyzed for insights. Hospitals can track trends, like the number of visits for specific conditions, treatment outcomes, or readmission rates, and use that data for strategic decisions or compliance reporting.
Every EMR system must follow strict compliance standards like HIPAA to ensure patient privacy. Role-based access controls, encryption, and audit trails protect sensitive information from unauthorized use or breaches.
Whether it’s a small clinic looking for a lightweight platform or a large healthcare network requiring deep integrations, our EMR development ensures smooth workflows, secure data management, and a user-friendly experience for clinicians.
Developing an EMR system tailored to your healthcare organization can change how efficiently you operate day to day. Beyond just digitizing patient records, EMR software can streamline operations, reduce costs, and improve care quality. Here are the most significant advantages:
EMR systems automate many repetitive and time-consuming administrative tasks, like filing, chart retrieval, and manual updates. This gives healthcare staff more time to focus on patients rather than paperwork.
From appointment scheduling to test result management, every process becomes faster and more organized.
Manual data entry and handwritten notes often lead to miscommunication or prescription errors. EMR software minimizes those risks through standardized templates, automatic checks for drug interactions, and clinical alerts.
Accurate, real-time data ensures that every healthcare decision is based on reliable information.
Though initial setup and training can require investment, EMRs significantly reduce long-term costs. They eliminate the need for physical storage, cut down on administrative overhead, and help avoid duplicate tests or treatments.
In the long run, these efficiencies contribute to a measurable ROI for healthcare providers.
With all patient data centralized and instantly accessible, collaboration between doctors, nurses, and lab technicians improves. Everyone can see the same patient information, lab results, and updates, which means fewer delays and fewer misunderstandings.
Patients today expect convenience and transparency. EMR systems often include patient portals that let individuals view their records, request refills, and track their medical history.
When patients can access their own data, they’re more likely to follow treatment plans and stay consistent with follow-ups.
Whether for research, compliance, or performance review, EMR systems make it easy to search and extract specific patient or operational data. Quick access to these insights supports decision-making and helps maintain regulatory compliance.
Modern EMR systems are designed to grow with your organization. They can integrate with laboratory systems, billing tools, and external healthcare apps, forming the foundation for larger digital ecosystems like EHRs or telemedicine platforms.
In short, EMR software development isn’t just about modernization; it’s about building an operational backbone that supports long-term efficiency, accuracy, and quality of care.
From an EHR vs EMR development perspective, EHR software goes beyond record-keeping. It connects entire healthcare ecosystems, enabling collaboration, compliance, and scalability. By enabling data exchange across hospitals, clinics, labs, pharmacies, and even insurance systems, EHRs ensure that everyone involved in patient care is on the same page. Here are some of the top ways healthcare providers use EHR systems to deliver smarter, coordinated care.
EHRs consolidate data from multiple sources, primary care clinics, specialists, labs, and even wearable health devices, into a single, comprehensive profile.
This unified record gives healthcare providers a complete picture of the patient’s health history, improving diagnosis accuracy and treatment outcomes.
EHRs make it easier for multiple care providers to collaborate. For example, if a cardiologist and a primary care physician are both managing the same patient, they can access and update the same record in real time.
This reduces duplicate tests, prevents conflicting treatments, and ensures that all clinicians are working with the same up-to-date information.
Because EHRs collect large amounts of data across entire patient populations, they’re powerful tools for identifying public health trends. Healthcare organizations can track chronic disease patterns, vaccination rates, or emerging risks, and design preventive care strategies accordingly.
Modern EHR systems can integrate with telemedicine and remote patient monitoring (RPM) tools. Data from connected devices, such as blood pressure monitors or glucose trackers, flows directly into the EHR, allowing doctors to monitor patients outside the clinic.
This is particularly valuable for managing chronic conditions and reducing unnecessary hospital visits.
EHRs enable healthcare providers to turn raw patient data into actionable insights. Hospitals can analyze treatment outcomes, readmission rates, and resource utilization to improve performance and decision-making.
In public healthcare systems, these analytics also support policy planning and health research.
Most EHRs include patient portals that let individuals access their medical records, view lab results, schedule appointments, and communicate securely with their doctors.
This transparency helps patients become active participants in their own care, fostering trust and accountability.
EHRs can connect to pharmacy networks, imaging centers, and insurance databases through interoperability standards like HL7 and FHIR.
This ensures that prescription orders, insurance claims, and medical images can all be accessed and updated without manual intervention, saving time and reducing administrative errors.
EHR systems, when implemented correctly, serve as the central nervous system of healthcare operations.
They link every piece of the patient journey, from diagnosis to recovery, making healthcare more connected, data-driven, and patient-centered.
Developing a customized EHR system gives healthcare organizations control, flexibility, and scalability that off-the-shelf software can’t match. The right EHR solution connects every part of a healthcare network, clinical, administrative, and analytical, into one intelligent system. Here are the core advantages of investing in EHR software development.
EHR software allows data to move freely between hospitals, clinics, laboratories, pharmacies, and insurance providers. When every stakeholder can access accurate, updated patient information, it reduces redundancies and improves care continuity.
For example, a specialist can instantly view lab results ordered by a general practitioner instead of repeating tests, saving time, cost, and patient frustration.
EHR systems give healthcare professionals a complete view of a patient’s history, diagnoses, past treatments, allergies, and medications. This context helps them make faster, safer, and more informed decisions.
When doctors can see everything in one place, it reduces the risk of conflicting treatments and ensures personalized, evidence-based care.
Beyond clinical use, EHRs generate valuable data that can be analyzed to identify trends, inefficiencies, and outcomes. Hospitals can use these insights to improve operations, measure physician performance, and enhance patient satisfaction.
At a larger scale, health authorities can leverage aggregated EHR data for research, policy planning, and disease prevention initiatives.
Patients can log in to portals linked to the EHR to view their medical history, test results, and upcoming appointments. Some systems also allow direct messaging with healthcare providers.
This access empowers patients to take charge of their health, adhere to treatment plans, and feel more connected to their care journey.
Healthcare data is sensitive, and EHR systems must meet strict compliance standards such as HIPAA, GDPR, or local health data regulations.
Modern EHR solutions include role-based access control, audit trails, and end-to-end encryption to ensure that patient data remains confidential and tamper-proof.
Custom EHR platforms can evolve with your organization. Whether you expand your facilities, adopt telehealth, or integrate new diagnostic tools, a well-architected EHR adapts seamlessly.
Developing your own system also gives you the freedom to add new modules or AI-driven capabilities as technology advances.
By eliminating paperwork, minimizing manual errors, and streamlining administrative tasks, EHRs save substantial time and money. Automated workflows, like patient check-ins, record updates, and billing, reduce operational costs while improving accuracy and speed.
With all medical data stored in one place and updated in real time, multiple providers can collaborate effectively. Whether it’s a general practitioner consulting with a specialist or a hospital coordinating with an external lab, EHRs keep everyone aligned and informed.
In essence, EHR software development is about creating a digital backbone that supports every clinical and administrative process. It turns healthcare data into a powerful asset, one that fuels better decisions, stronger collaboration, and improved patient care.
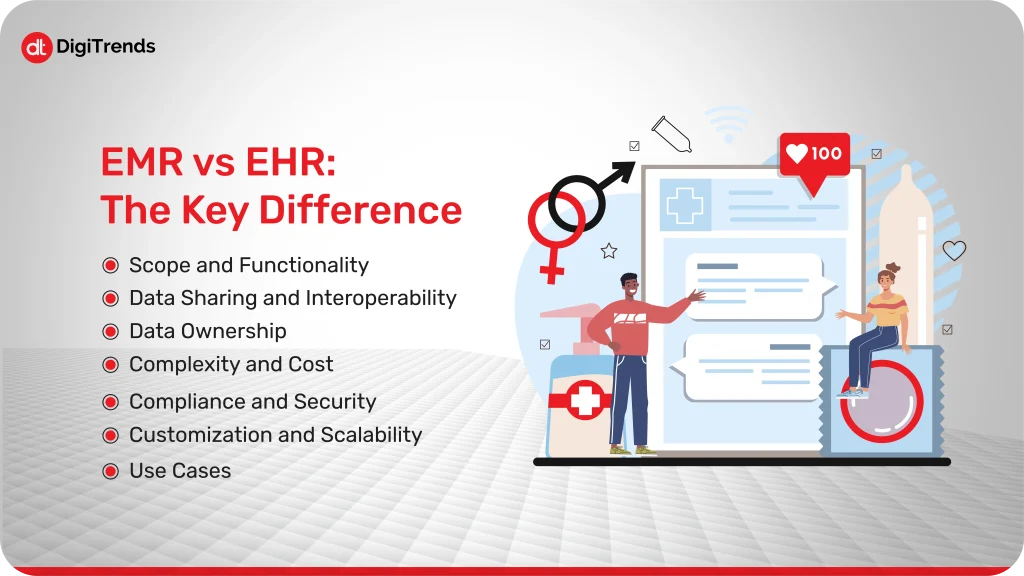
The terms EHR and EMR are often used interchangeably, but they’re not the same thing. Both systems digitize medical data, yet they differ in purpose, scale, and functionality. Understanding these distinctions is crucial before deciding which one fits your healthcare business.
Let’s break it down clearly.
EMR: Focuses on managing patient records within a single healthcare organization, like a clinic, hospital department, or private practice. It includes diagnoses, prescriptions, and lab results, but stays confined to that facility.
EHR: Goes beyond one organization. It integrates patient data from multiple providers, creating a complete medical history accessible across healthcare networks.
In short, EMR is about your patients, while EHR is about the patient’s health journey everywhere.
EMR: Limited interoperability. Data doesn’t move automatically to external systems; it usually needs manual export or printouts.
EHR: Designed for interoperability. It connects hospitals, labs, and pharmacies, ensuring smooth data exchange through standards like HL7 and FHIR.
Verdict: EHRs enable collaboration and coordinated care; EMRs mainly serve internal operations.
EMR: The data belongs to the healthcare provider or organization maintaining the system.
EHR: Patients typically have access to and some control over their health information through secure portals.
This gives EHRs an edge in patient empowerment and transparency.
EMR: Simpler and cheaper to implement. Ideal for smaller practices with limited IT budgets and internal data needs.
EHR: More complex, requiring advanced infrastructure, integrations, and compliance measures. Suitable for large hospitals or networks managing diverse care services.
Both EMR and EHR systems must adhere to healthcare data regulations like HIPAA or GDPR.
However, EHRs usually demand stronger security frameworks since they involve cross-organizational data sharing and patient access.
EMR: Built around the needs of a specific practice, efficient but not easily scalable.
EHR: Designed to grow and integrate with other systems over time, supporting expansion and digital transformation efforts.
| Category | EMR | EHR |
| Ideal For | Small to mid-size clinics | Large hospitals, healthcare systems |
| Focus | Internal patient record management | Cross-organization data exchange |
| Interoperability | Limited | High |
| Patient Access | Usually none | Yes, visa portals |
| Scalability | Moderate | Extensive |
| Compliance | HIIPAA, GDPR | HIPAA, GDPR, and advanced interoperability standards |
Both systems serve different stages of healthcare digital transformation. EMRs often come first; EHRs follow as organizations expand and integrate.
Choosing between EHR and EMR isn’t about which system is “better.” It’s about what your healthcare organization needs, today and in the future. Each solution has its own advantages, but the right choice depends on your goals, scale, and how connected you want your operations to be.
Let’s walk through how to decide.
If your organization is a single clinic, diagnostic lab, or small practice, an EMR system is usually enough. It simplifies record-keeping, streamlines workflows, and improves internal communication, all without the cost or complexity of a fully connected system.
But if you manage multiple locations, collaborate with external partners, or want to share patient data across networks, an EHR system is the smarter long-term investment. It’s designed for interoperability and growth.
One of the most common mistakes healthcare organizations make is choosing an EMR just to “go digital,” then realizing a few years later that they’ve outgrown it.
If expansion, partnerships, or integrations with telemedicine platforms are on your roadmap, you’ll eventually need the flexibility of an EHR. Developing an EHR from the start ensures you’re building on a scalable foundation.
Both systems must follow healthcare data regulations like HIPAA or GDPR, but the level of compliance differs.
If you need to exchange patient data between facilities, pharmacies, or labs, you’ll need an EHR that supports interoperability standards such as HL7, FHIR, and C-CDA.
For single-practice setups where data stays internal, EMRs provide sufficient protection without the added complexity.
EHR development and implementation demand more robust IT infrastructure, integration expertise, and ongoing maintenance.
If your organization lacks these resources, starting with a simpler EMR can be a cost-effective way to digitize records, improve workflows, and build digital readiness before scaling up to a full EHR later.
Patients today expect transparency, accessibility, and digital convenience. EHR systems with patient portals give them direct access to their health data, appointments, and test results, building trust and engagement.
If patient engagement and care coordination are strategic goals, an EHR delivers stronger long-term value.
EHRs support multi-department, multi-location operations, ideal for hospitals or healthcare systems.
EMRs are best for focused workflows, such as general practitioners or specialist clinics that operate independently.
If your workflow involves data exchange between multiple entities, choose EHR. If it’s confined within your team, EMR fits better.
Ask whether you will need to connect your system with lab software, imaging tools, telemedicine platforms, or billing systems.
If yes, you’ll need an EHR architecture that allows seamless API integration and future expansion.
| Scenario | Recommended Solution |
| Single clinic or small practice | EMR |
| Large hospital or multi-branch network | EHR |
| Collaboration with labs or pharmacies | EHR |
| Focus on internal efficiency | EMR |
| Focus on data sharing and scalability | EHR |
| Limited IT resources and budget | EMR |
Both play vital roles in healthcare digital transformation. The key is choosing the one that aligns with your organization’s maturity, resources, and strategic direction.
Choosing between EHR and EMR is only part of the journey. The real difference comes from how well your system aligns with your workflows, goals, and compliance needs. That’s where DigiTrends comes in.
We build custom healthcare software that’s secure, scalable, and designed for real-world use. Whether you’re exploring EHR vs EMR development, our team builds healthcare software tailored to your operations and compliance needs.
Our development process focuses on interoperability, compliance, and usability. Every system we create follows standards like HIPAA, GDPR, FHIR, and HL7, ensuring data moves safely and seamlessly across your healthcare ecosystem.
We design interfaces that are intuitive for doctors, nurses, and staff, with clean layouts, fast workflows, and minimal clicks. Our goal is simple: make technology an enabler, not an obstacle.
And once your system is live, we stay with you. From integration and maintenance to adding new features like AI analytics or telehealth modules, we help your healthcare business stay ahead of change.
If you’re ready to build or upgrade your digital health platform, let’s talk. DigiTrends can help you create healthcare technology that’s secure, efficient, and future-ready.