
Voice Recognition Technology in Healthcare: Benefits for Patients and Providers
Explore how voice recognition technology is being used across healthcare and the role of voice assistants in clinical environments.
Continue Reading
GCC regions like Saudi Arabia, the UAE, and Qatar are going through a major digital transformation of the healthcare industry. Governments are actively working towards achieving a digital-first healthcare approach, automating and modernizing hospital systems. This digital economy push is also leading new telemedicine and remote patient monitoring platforms to enter the Middle Eastern market.
If you are a leading hospital or clinic network in the Middle East considering to develop a healthcare software, there is one thing that matters the most, and that is:
Whether the investment you make today will work well with the evolving regulations, growth, and operational challenges in the future.
Now that we have entered 2026, questions around development budget matter a lot as they change with multiple factors including time, growth, operational requirements, and more. If you are building healthcare software in the Middle Eastern regions like Saudi Arabia, the UAE, and Qatar, then you would not only have to consider the development hours required to have an idea of the costs, there are many other areas to consider to have a proper understanding of the expected budget including design, complexity, features, integrations, etc.
Healthcare software development cost in the Middle East now highly depend on multiple factors like regulatory requirements, data hosting laws, security standards, and the growing expectation for scalable, patient-centric digital experiences. Furthermore, different healthcare platforms have different pricings, as it all comes down to where and how they are built.
If you are a healthcare provider, founder, or decision-maker looking for clear factors of price before investing, this blog is your best bet. We will break down what goes into healthcare software development costs in the Middle East, what drives prices up or down, and how businesses can plan smarter in 2026 without cutting corners on compliance or quality.
Traditional healthcare platforms are now being replaced with smarter systems with the help of new technologies like artificial intelligence, cloud computing, etc.
Due to the increasing adoption of technology in the healthcare industry, healthcare software development is going through a major change, as patients now expect intelligent systems, faster processes, and digital access to services.
As patients have begun to actually expect platforms to deliver smart and automated systems, healthcare providers, startups, and companies are actively investing in medical software development and adopting modern solutions for patient care like remote patient monitoring, electronic health records (EHRs), and AI-powered diagnostic tools. According to recent research, the Middle East’s healthcare IT market is poised to reach $7.9 billion by 2028.
These numbers depict the growth and the shift in the way healthcare is provided to patients. Patients now expect healthcare platforms to provide smoother processes and easy access to services, which directly affects the cost of healthcare software development. If you are looking to build healthcare software, you will have to consider patients’ expectations and prioritize long-term scalability, seamless integration, and regulatory readiness in your digital strategies.
Right now, the numbers suggest that the market is in a great position to enter the healthcare software market for your hospital, startup, or healthcare organization in the Middle East.
Healthcare software development costs in the Middle East vary widely, depending on what you’re building, where it’s being deployed, and how strictly it needs to align with regional regulations. In 2026, the region sits in a unique position: more affordable than the US and Western Europe, but more structured and compliance-driven than offshore markets.
Let’s break it down clearly.
Different healthcare solutions come with very different cost profiles. Here’s what organizations typically budget for custom development in the Middle East.
| Software Type | Cost Range (USD) | Cost Range (AED) | Description |
| Basic mHealth App | $30,000 – $60,000 | AED 110,000 – AED 220,000 | Appointment booking, patient profiles, basic dashboards |
| Telemedicine Platform | $60,000 – $150,000 | AED 220,000 – AED 550,000 | Video consultations, chat, e-prescriptions, and scheduling |
| EHR/EMR System | $120,000 – $300,000 | AED 440,000 – AED 1,100,000 | Interoperability, audit logs, and role-based access |
| Remote Patient Monitoring | $150,000 – $350,000+ | AED 550,000 – AED 1,285,000+ | IoMT integrations, real-time alerts, analytics |
| Hospital Management System | $250,000 – $500,000+ | AED 920,000 – AED 1,835,000+ | Multi-department workflows, reporting, and integrations |
| AI-Powered Healthcare Software | $300,000+ | AED 1,100,000+ | Diagnostics, predictive analytics, clinical decision support |
These estimates reflect custom-built, compliance-ready solutions, not off-the-shelf products with limited flexibility.
These countries are often grouped when it comes to costs, but healthcare software development costs differ due to different regulatory frameworks, hosting requirements, and system maturity. Let’s have a look:
| Country | Relative Cost Level | Key Cost Drivers |
| UAE | Medium – High | Data protection laws, cloud compliance, and high UX standards |
| Saudi Arabia | High | PDPL, NPHIES integration, local data hosting, national health programs |
| Qatar | Medium – High | Government-led healthcare, enterprise security standards |
In Saudi Arabia, the costs of healthcare software development are relatively higher than the costs in Qatar and the UAE because the platforms are required to align with the national healthcare infrastructure and strict data residency rules. UAE projects can prove to be a little more complex comparatively, as they are more focused on security, scalability, and patient experience, which also pushes the costs. The Qatar market size is smaller than the other two others but high standards for healthcare software used by public and private entities are maintained.
The healthcare software development cost in the Middle East differs from the costs in the USA and Western Europe; it is more affordable.
But why this much difference?
The reason healthcare software development costs are higher in the USA and Western Europe than in the Middle East is due to high labor costs, long certification procedures, and legacy system constraints that directly push the budget.
The costs might be lower than the development costs in the USA and Western Europe, but are still higher than the development costs in low-cost countries. This is because digital healthcare platforms in the Middle East are required to comply with strict regulatory expectations, enterprise-grade security standards, and often require local hosting and interoperability with national health systems.
What this means is that healthcare software development in the Middle East is about balance. It is cost-efficient, but there is no compromise on the quality, compliance, and scalability. If you are looking to build healthcare software in the Middle East, you have chosen the right path, as 2026 strategically sounds like a good year to build scalable, long-term healthcare software.
Sometimes healthcare software development budgets go off track, and this is usually because teams are not fully aware of the factors where the money will go beforehand.
Development isn’t just about coding; it requires several steps that are closely tied together as one depends on the other, and all the factors deployed affect the costs. It is important to understand the costs of each step so you can set realistic budget expectations and avoid surprises later.
UI and UX are not just about how the software looks. In healthcare, design directly affects usability, adoption, and patient safety. This phase includes user research, journey mapping, wireframes, and accessibility planning for both patients and clinicians.
In the Middle East, healthcare platforms are expected to support multilingual users, clear workflows, and intuitive navigation. These requirements push design costs higher than standard apps, but significantly reduce training and support costs later.
Typical cost share: 10–15% of the total project budget
This is where most of the budget is allocated. Backend development covers databases, APIs, business logic, and system architecture. Front-end development focuses on web or mobile interfaces used by patients, doctors, and administrators.
Healthcare software often requires complex role-based access, real-time data handling, and high availability. These requirements increase development time and cost, especially for enterprise or hospital-grade systems.
Typical cost share: 40–50% of the total project budget
Integrations are one of the biggest cost variables in healthcare projects. Connecting with EHR or HIS platforms, medical devices, wearables, laboratories, insurance systems, or payment gateways requires custom logic and extensive testing.
In the Middle East, integration with national health systems or approved vendors adds another layer of complexity. Each integration increases both development and long-term maintenance costs.
Typical cost share: 15–25% of the total project budget
Security is not optional in healthcare. This phase includes encryption, secure authentication, audit logs, access controls, and data protection mechanisms aligned with regional regulations.
Middle Eastern healthcare platforms often require local data hosting, strict access governance, and compliance-ready security architecture from day one. Skipping or underestimating this stage leads to costly rework and compliance risks.
Typical cost share: 10–15% of the total project budget
Healthcare software must be tested beyond basic functionality. This includes performance testing, security testing, interoperability testing, and user acceptance testing for clinical workflows.
If the software falls under regulated categories, additional effort is required for documentation and certification readiness. This phase ensures reliability, safety, and regulatory alignment before launch.
Typical cost share: 10–15% of the total project budget
Launching healthcare software is only the beginning. Deployment includes cloud setup, environment configuration, and go-live support. Ongoing maintenance covers updates, security patches, performance optimization, and scalability planning.
In the Middle East, systems are often designed to scale across facilities, regions, or patient populations. Planning for growth early avoids expensive architectural changes later.
Typical cost share: 10–20% annually after launch
What this really means is simple. Healthcare software costs are not driven by development alone. They’re shaped by compliance, integrations, security, and long-term scalability. A realistic cost breakdown helps organizations invest wisely and build platforms that last rather than cutting corners that cost more later.
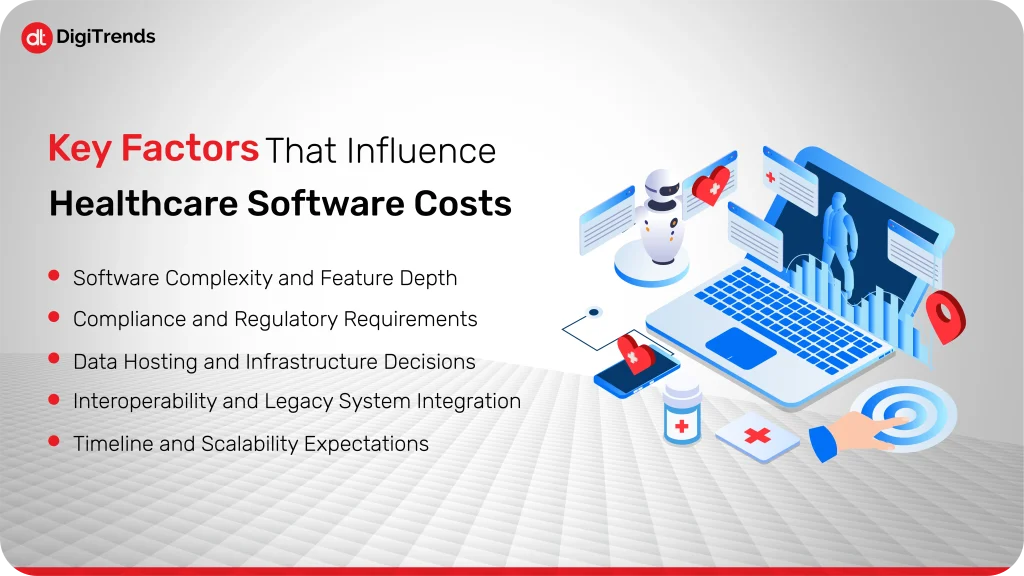
Healthcare software pricing isn’t fixed. Two platforms that look similar on the surface can have very different costs once you factor in regulations, integrations, and long-term expectations. In the Middle East, these variables play an even bigger role because healthcare systems are tightly regulated and built for scale.
Here are the factors that most directly influence cost.
The more the software does, the more it costs. A simple appointment booking app is very different from a platform that includes real-time monitoring, clinical dashboards, AI-driven insights, and multi-role access.
Features like e-prescriptions, video consultations, analytics, and automated workflows add layers of logic and testing. As feature depth increases, so do development time, QA effort, and long-term maintenance costs.
Compliance is one of the biggest cost drivers in healthcare software. Meeting standards like HIPAA, GDPR, or regional healthcare regulations requires secure architecture, detailed documentation, and rigorous testing.
In the Middle East, regulations often include local data residency, patient consent management, and integration with national health systems. These requirements increase development effort but are non-negotiable for market entry.
Where and how data is hosted has a direct impact on cost. Cloud-based infrastructure offers flexibility and scalability, but regional regulations may require local or government-approved hosting providers.
On-premise or hybrid setups increase upfront costs and operational overhead. Infrastructure decisions also affect performance, disaster recovery, and long-term scalability, all of which influence the total cost of ownership.
Healthcare environments rarely operate in isolation. New software often needs to integrate with existing EHRs, hospital information systems, laboratory systems, or medical devices.
Legacy systems can be difficult to integrate due to outdated standards or limited documentation. Each integration increases development time, testing requirements, and ongoing support costs, especially in large hospital networks.
Shorter timelines usually mean higher costs. Accelerated development requires larger teams, parallel workflows, and extended testing cycles.
Scalability expectations also matter. Software built to support one clinic is far less complex than software designed to scale across multiple facilities or regions. Planning for growth upfront adds to initial costs but prevents expensive rework later.
What this really comes down to is planning. Healthcare software costs rise when complexity, compliance, and scalability are underestimated. Clear requirements, realistic timelines, and early architectural decisions make the difference between controlled investment and runaway budgets.
Before we dive straight into the healthcare software development services and technologies, you should know what benefits they provide to patients and healthcare providers.
Let’s have a look at the benefits of healthcare software development:
Healthcare software now comes with features like AI-powered diagnostics, telemedicine, and remote patient monitoring, which allows patients to receive faster and more effective care, as this software provides accurate diagnoses, real-time monitoring, and personalized treatment plans for patients. Imagine receiving accurate diagnoses for your illness and getting prescribed medicines and treatment faster than physically visiting a doctor for non-critical issues like the flu. It’s great, right? This is one of the benefits of digital healthcare.
We all have seen how busy the hospital systems are. Sometimes the staff makes mistakes, writes the wrong names, or files are lost. A healthcare software will solve all these issues by streamlining administrative workflows and automating appointment scheduling, billing, patient data management, and reporting. This will reduce paperwork, manual errors, and save time for both healthcare staff and patients.
With technologies like AI/ML or AR/VR being added in healthcare software, doctors can study the patient’s body in a better way, which will lead to a fast and efficient diagnosis for critical cases, especially. Advanced analytics and integrated dashboards will give healthcare providers a 360-degree view of patient history, treatment effectiveness, and resource utilization. These insights will help them make evidence-based decisions, and the results will be improved, too.
From mobile apps to patient portals, healthcare software allows patients to track their health, communicate with doctors, and access records at their convenience, which builds trust, and patients will more frequently get checkups and treatment because of its accessibility.
For a business or healthcare provider looking to scale up the healthcare business or even a startup looking to build something meaningful, medical software development is the right option as it is a highly scalable business due to its increasing demand, and the software can also be integrated into hospital systems, IoT devices, or third-party services.
A custom healthcare software is the best option as it will reduce inefficiencies, minimize maintenance issues, and deliver a better return on investment. The cost of building it might be high, but it is completely worth it.
Custom healthcare software is a strategic asset that empowers providers to deliver smarter care, stay competitive, and adapt to an increasingly digital-first healthcare landscape.
The evolution of healthcare software is fueled by a powerful tech stack designed to handle everything from patient data and diagnostics to real-time communication and compliance. Here are the core technologies driving innovation in this space:
Artificial intelligence algorithms enable predictive analytics, medical image recognition, patient risk scoring, and even clinical decision support. ML models can be trained to detect anomalies in X-rays, predict disease progression, and personalize treatment recommendations. The use of AI in healthcare is increasing day by day and the market is projected to reach USD 504.17 billion by 2032.
IoMT is connected to devices like smart wearables, ECG monitors, and remote sensors that collect real-time patient data, which is then synced with apps or dashboards. These insights are critical for proactive care, chronic disease management, and remote monitoring.
Cloud-based platforms ensure secure storage, easy access, and scalable infrastructure for large volumes of healthcare data. They also support seamless integration with EHR systems, mobile apps, and telemedicine platforms, while offering cost-efficient deployment.
Blockchain adds transparency and security to health data management. It ensures immutable medical records, secure transactions, and improved traceability for items such as drug supply chains, patient consent, and health insurance claims.
Healthcare generates vast amounts of structured and unstructured data. Big Data platforms process this information to uncover patterns, improve diagnostics, reduce readmissions, and optimize hospital resource utilization.
Telemedicine app development includes secure video conferencing APIs, encrypted communication protocols, and virtual care platforms that are crucial to remote consultations, follow-ups, and mental health services, particularly in the post-COVID-19 era.
Mobile health apps enable patients to track fitness, medication schedules, or vital signs. Integration with wearables like Apple Watch or Fitbit enriches health data and encourages continuous engagement.
RPA (Robotic Process Automation) tools help healthcare providers automate repetitive administrative tasks such as billing, appointment reminders, insurance verification, and patient onboarding, freeing up valuable human resources.
To ensure interoperability and regulatory compliance in healthcare software, developers implement standards like FHIR (Fast Healthcare Interoperability Resources) and HL7, which facilitate secure data exchange across healthcare systems.
Modern healthcare software isn’t built with just one technology; it’s the result of a carefully orchestrated tech stack that blends data, connectivity, and intelligence. Choosing the right technologies can make the difference between a basic app and a high-impact healthcare solution.
Healthcare software development covers a wide range of services tailored to meet the needs of hospitals, clinics, startups, insurers, and other healthcare providers. These are the most in-demand and impactful services offered by development companies today:
Tailored solutions built from the ground up to meet specific business and clinical requirements. These can include EHR systems, diagnostic tools, hospital management platforms, or specialized patient apps, designed to be fully scalable, secure, and user-friendly.
Development of robust, interoperable platforms like electronic health records (EHR) or electronic medical records systems (EMR) for managing patient medical history, treatment plans, and diagnostics. Includes integration with third-party systems, compliance with HIPAA/HL7/FHIR, and role-based access control.
Creation of secure, user-friendly platforms that enable virtual consultations, remote diagnosis, follow-up care, and even mental health services. Often includes features like real-time video/audio, e-prescriptions, appointment scheduling, and in-app payments.
Mobile health apps that empower patients to monitor vitals, manage medications, access health records, and interact with healthcare providers on the go. Includes integration with wearable devices and adherence to medical app regulations.
Development of CRMs focused on patient relationship management, tracking patient journeys, personalizing communication, automating reminders, and optimizing marketing or engagement campaigns.
Custom software that automates and optimizes billing, claims processing, and insurance verification. Designed to reduce errors, prevent claim rejections, and improve financial performance for healthcare providers.
Software that collects and analyzes real-time patient health data (e.g., heart rate, glucose levels) from IoMT devices and sends alerts to care teams if intervention is needed. Vital for chronic condition management and post-operative care.
Advanced dashboards and data platforms that enable predictive analytics, operational reporting, population health management, and clinical decision support.
Connecting new solutions with legacy systems like HIS (Hospital Information Systems), PACS, LIS, pharmacy databases, or insurance platforms, ensuring seamless data flow and unified workflows across departments.
From mobile apps that engage patients to backend systems that streamline hospital operations, these services form the foundation of digital healthcare transformation. Choosing the right mix of services depends on your specific goals, whether it’s improving care delivery, boosting patient engagement, or increasing operational efficiency.
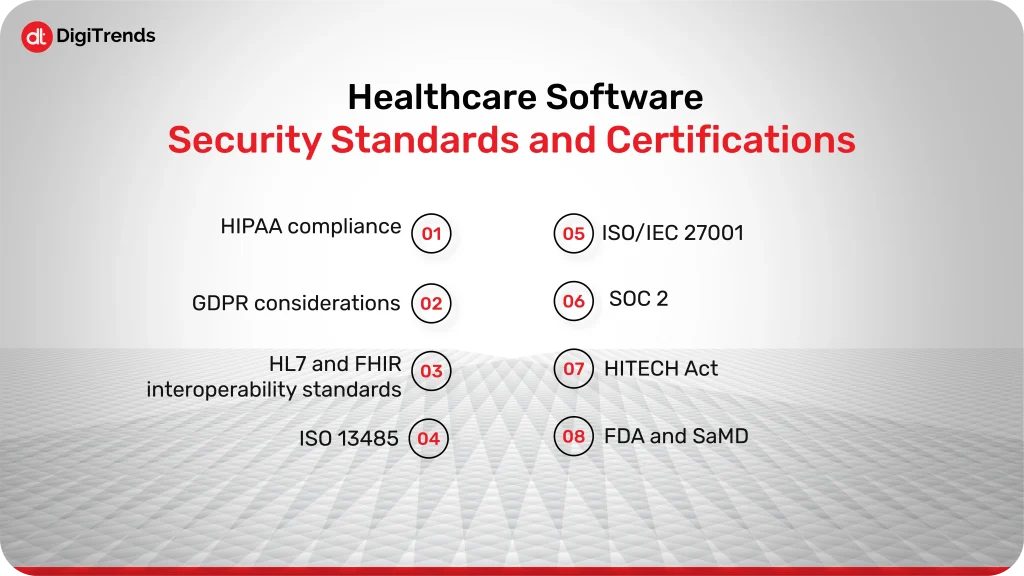
Security in healthcare software is not a feature. It’s a baseline requirement that directly affects cost, timelines, and system architecture. In regulated environments, every certification adds effort, documentation, and validation, but skipping them isn’t an option.
HIPAA requires strict controls around patient data, including encryption, access management, and audit logs. Implementing these safeguards adds development and testing effort, but it also reduces long-term risk and rework. For platforms serving US-linked providers or partners, HIPAA compliance is unavoidable.
Healthcare software handling data from EU citizens must support consent management, data access requests, and deletion workflows. These requirements influence database design, user flows, and backend logic, increasing development scope even for Middle East–based platforms.
HL7 and FHIR enable secure data exchange between healthcare systems. Implementing these standards increases upfront development cost but is essential for interoperability with EHRs, national health systems, and third-party providers.
For software classified as Software as a Medical Device, ISO 13485 introduces quality management processes that impact how software is designed, tested, and documented. This standard adds structure and cost but is critical for regulated clinical applications.
ISO/IEC 27001 focuses on organization-wide information security practices. Achieving alignment often requires changes beyond code, including infrastructure policies and risk management processes, which influence both development and operational costs.
SOC 2 is particularly relevant for cloud-based healthcare software. Meeting its requirements involves strong access controls, monitoring, and operational discipline, all of which increase development and compliance overhead.
HITECH strengthens HIPAA enforcement and increases penalties for breaches. From a cost perspective, this pushes teams to invest more in security testing, monitoring, and incident response planning.
Software that supports diagnostics or treatment decisions may require FDA clearance. This process demands extensive documentation, validation, and risk assessment, significantly impacting timelines and budgets.
Middle Eastern healthcare regulations are shaping how software is built, hosted, and maintained. Compliance here isn’t generic; it’s country-specific and tightly enforced.
Saudi Arabia requires strict data protection under PDPL and mandates integration with NPHIES for healthcare transactions. These requirements influence architecture decisions, data hosting, and integration costs from day one.
The UAE enforces clear rules around patient data privacy, access control, and secure hosting. Healthcare software must align with federal and emirate-level regulations, increasing compliance planning and validation efforts.
Many Middle East healthcare platforms must use approved or local cloud providers. This limits infrastructure choices and often increases hosting and operational costs compared to unrestricted global cloud deployments.
Compliance adds checkpoints throughout the development lifecycle. Architecture reviews, security audits, and validation cycles extend timelines but reduce the risk of costly delays or rework after launch.
Lowering costs in healthcare software isn’t about cutting corners. It’s about making smarter decisions early.
Modular architecture allows teams to add features over time without rebuilding core systems. This reduces upfront cost while keeping future expansion affordable.
Launching with essential features helps validate the product without overinvesting early. Additional capabilities can be introduced once the platform proves its value.
Designing for compliance from the start avoids expensive redesigns later. Security-first architecture may cost more upfront, but it saves time and money long-term.
Clear requirements, realistic timelines, and early stakeholder alignment prevent scope creep and unexpected rebuilds, which are among the biggest budget killers in healthcare projects.
DigiTrends partners with healthcare providers and healthtech startups to design and build digital solutions that align with regional healthcare requirements and long-term business goals. With experience across multiple healthcare domains, the focus remains on delivering software that is reliable, compliant, and built for real-world use.
With region-specific healthcare expertise, DigiTrends understands the regulatory landscape, data privacy expectations, and system integration standards across markets such as Saudi Arabia and the UAE. This regional understanding helps ensure that healthcare platforms are designed in line with local operational and compliance needs.
Healthcare software development in the Middle East is a serious investment, not an experimental one. Costs are shaped by compliance, security, integrations, and long-term scalability, not just development effort.
For decision-makers, the key takeaway is simple: early planning reduces long-term expenses. Clear requirements, realistic budgets, and compliance-ready architecture make the difference between sustainable platforms and costly rework.
As digital healthcare continues to expand across the region, organizations that approach software development strategically will be better positioned to scale, adapt, and deliver meaningful patient outcomes in 2026 and beyond.