Voice Recognition Technology in Healthcare: Benefits for Patients and Providers
Explore how voice recognition technology is being used across healthcare and the role of voice assistants in clinical environments.
Continue Reading
Virtual reality (VR) is transforming the healthcare landscape by providing immersive and interactive experiences that enhance medical education and patient care. This technology, once limited to gaming and entertainment, has evolved into a powerful tool enabling healthcare professionals to train more effectively, enhance patient outcomes, and expand access to care. According to recent research, the global virtual reality in healthcare market is projected to be valued at USD 46.37 billion by 2032.
Explore what VR in healthcare is, its benefits, practical use cases, implementation challenges, future trends, and answers to frequently asked questions.
Virtual reality in healthcare involves the use of computer-generated three-dimensional environments that healthcare professionals and patients can interact with in real time. Using specialized headsets, motion sensors, and software, VR creates an immersive simulation that replicates medical scenarios, anatomy, or therapeutic environments. This can range from non-immersive screen-based applications to fully immersive VR experiences requiring advanced hardware.
The unique characteristic of VR is its ability to offer realistic, hands-on practice without involving any risk to real patients. For medical students and professionals, this means practicing surgeries or emergency scenarios repeatedly to refine their skills. For patients, it provides therapeutic environments for pain distraction, mental health therapy, or physical rehabilitation. In essence, VR bridges the gap between theoretical knowledge and real-world application by delivering controlled, repeatable, and adaptable experiences.
VR revolutionizes medical education by enabling students and practitioners to engage in lifelike simulations. It allows medical professionals to practice complex surgeries and procedures multiple times, gaining familiarity and confidence without the pressure or risk of harming a patient. Medical students can explore anatomy through 3D visualization, far surpassing traditional textbook methods and allowing for interactive learning.
Besides technical skills, VR platforms simulate patient interactions, teaching empathy, communication, and critical thinking. Moreover, VR facilitates remote training, connecting students worldwide with experts through interactive classrooms and mentoring. This democratizes medical education and ensures high standards globally.
Patients benefit enormously from VR applications, especially in pain management and rehabilitation. Immersive VR environments distract patients during painful procedures, reducing perceived pain and anxiety. Such non-drug interventions are increasingly valuable amid concerns over opioid use.
Physical rehabilitation programs use gamified VR exercises, boosting patient engagement and adherence. Virtual environments motivate patients to complete therapy sessions actively, accelerating recovery for stroke, injury, or chronic conditions. VR also supports mental health treatments such as exposure therapy for anxiety, PTSD, and phobias by creating controlled, therapeutic simulations.
VR lowers barriers to healthcare access by enabling remote therapeutic sessions and consultations, particularly beneficial for patients in rural or underserved areas. This reduces travel needs and optimizes healthcare delivery.
Financially, VR decreases training costs by supplementing traditional methods and minimizing errors through better preparation. Accelerated patient recovery, thanks to engaging therapy, also reduces overall healthcare expenses.
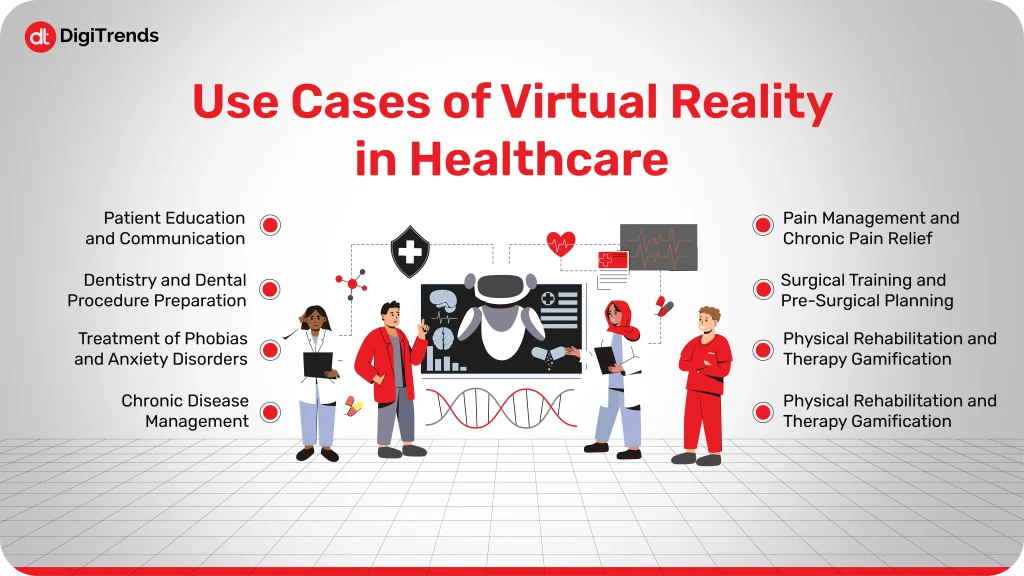
VR provides distraction therapy, significantly reducing acute and chronic pain during procedures like burn care, dentistry, or chemotherapy. It improves patients’ comfort without added medications.
VR environments allow surgeons to practice intricate procedures repetitively, refining skills and decision-making. Personalized 3D models created from patient scans help pre-plan surgeries, improving precision and outcomes.
Rehabilitation programs using VR infuse fun and motivation into physical therapy. Patients perform interactive exercises tailored to their recovery needs, improving functional outcomes and compliance.
VR exposure therapy safely immerses patients in anxiety-provoking scenarios, helping them overcome phobias and PTSD. It also offers mindfulness environments to support stress and depression management.
Immersive VR tools educate patients by visually explaining conditions and treatments, fostering informed decision-making and trust between patients and providers.
VR familiarizes patients with dental treatments beforehand, decreasing anxiety and improving cooperation during procedures.
Through gradual exposure in virtual settings, patients desensitize to fears such as heights, social phobia, or spiders, reducing avoidance behaviors effectively.
Interactive VR modules guide patients through self-care practices for managing chronic illnesses like diabetes and cardiovascular diseases, promoting better health outcomes.
Healthcare facilities use a variety of VR hardware, including head-mounted displays (HMDs), handheld controllers, and haptic feedback devices that simulate touch. Software platforms provide realistic simulations for education, treatment, and rehabilitation.
VR integrates with other advanced technologies such as artificial intelligence (AI) and augmented reality (AR) to deliver personalized medicine. AI analyzes patient data in real time to modify VR therapeutic environments or provide tailored training feedback.
Clinical implementation spans hospitals, outpatient centers, physical therapy clinics, and remote care settings. Accessibility improvements continue with more affordable and portable VR devices, making adoption easier.
Despite its promise, VR adoption in healthcare faces several significant hurdles that must be addressed to fully realize its potential. One of the primary challenges is the high initial cost of hardware and software. Although prices for VR technology are gradually declining, many healthcare institutions, particularly smaller hospitals and clinics, still find the investment prohibitive. Besides the upfront equipment costs, maintaining and updating VR systems adds ongoing expenses. Technical issues such as motion sickness, system latency, limited battery life, and the need for frequent calibration can negatively impact the user experience, especially for patients who may already be vulnerable. These factors contribute to discomfort and reluctance among some users, hindering widespread acceptance.
Regulatory compliance is another critical barrier. Healthcare is a highly regulated industry, and VR applications must meet strict standards for patient safety, data protection, and efficacy to gain approval from authorities like the Food and Drug Administration (FDA) and equivalent bodies worldwide. Navigating these regulatory pathways can be lengthy and expensive, slowing down innovation and adoption.
Moreover, patient data privacy is a growing concern, especially as many VR systems collect sensitive health information and environmental data. Ensuring adherence to laws such as HIPAA in the U.S., implementing robust encryption, informed consent protocols, and third-party vendor risk management are essential but add layers of complexity to development and deployment.
Training healthcare staff in the effective use of VR tools is time-consuming and can face resistance. Many providers must learn to integrate VR technology seamlessly into clinical workflows while maintaining focus on patient care. This adjustment requires organizational commitment and ongoing education, which may strain already overburdened healthcare teams. Staff burnout and low retention rates compound this challenge, as ongoing training demands can overwhelm smaller or financially constrained facilities.
Patient acceptance varies significantly. While some patients embrace the immersive experience, others may feel skeptical or uncomfortable with new technology, especially elderly patients or individuals with sensory sensitivities. Issues like motion sickness or the psychological impact of immersive therapy need careful management. Consequently, building patient trust and ensuring clear communication about the benefits and risks of VR is vital.
Finally, the quality and realism of VR content continue to require improvement. For educational and therapeutic efficacy, VR scenarios must be highly accurate, detailed, and responsive. Insufficiently realistic simulations can diminish training effectiveness or therapeutic outcomes. As VR technology progresses, continuous investment in content development, usability enhancements, and user experience optimization is needed to maximize VR’s impact in healthcare settings.
Addressing these limitations requires coordinated efforts between technology developers, healthcare providers, regulators, and policymakers. With ongoing innovation and supportive frameworks, many of these challenges can be mitigated, enabling VR to fulfill its transformative promise in medicine.

The future of VR in healthcare is poised for expansion and deeper integration. Advances in hardware will enable more realistic haptic feedback and wireless experiences. AI-powered VR can offer dynamic, personalized training and treatments based on real-time biosensor data.
The widespread rollout of 5G networks will facilitate seamless remote VR consultations and surgeries, drastically enhancing telemedicine capabilities.
Extended reality (XR), combining VR, AR, and mixed reality, will enhance surgical precision with holographic anatomical overlays during operations. Gamified rehabilitation will become more engaging and patient-tailored, further improving adherence and outcomes.
Overall, VR and related technologies will become indispensable tools in healthcare, making treatments more effective, accessible, and personalized.
Virtual reality is transforming healthcare education, treatment, and patient engagement. As this technology advances, its integration promises more effective, accessible, and personalized care for everyone.